GM IRN GP & Researcher Collab Event
22.01.2026
Learn more about the Greater Manchester Inclusive Research Network here
Frontline practice teams serving deprived populations typically do not have the headspace to engage in research. Yet they bear witness to the impact of the wider determinants of health on a daily basis. This is the intersection at which we must develop and test healthcare interventions that work, for the communities that need them most. There has been a laudable drive to engage patients and the public in co-designing research. However a ‘PPIE equivalent’ for frontline teams serving deprived populations is long overdue.
We held our inaugural GM IRN GP & Researcher Collab Event on 22nd January 2026. There was a fantastic turnout, with over 115 colleagues from across GM and beyond joining us to help shape strategy for inclusive research in primary care. Hopefully, this is just the beginning of enduring connections and collaborations to drive inclusive, translational research from the frontline.
The event kicked off with our Founding Director, Dr Maria Ahmed Drake, who shared her powerful story of how personal tragedy has been the impetus for her mission to transform healthcare for underserved populations, through inclusive research and innovation. Dr Cordelle Ofori, Director of Public Health at Manchester City Council shared sobering insights into the stark health inequities that exist across GM and beyond and challenged us to adopt a whole-system approach to preventing ill-health. Prof Caroline Mitchell, co-Founder of the Sheffield DERA, expertly articulated how there is no health equity without research equity, reinforcing the need for frontline practice teams serving deprived populations to engage in research. Prof Peter Bower, Lead of the UoM Centre for Primary Care and Health Services Research spoke about the fantastic research infrastructure across GM and opportunities for frontline teams to pursue research. And the NW RRDN team, led by Susan Neeson, provided a wealth of information to support practices to become (more) research-active. Our Fireside Panel was chaired by the formidable Prof Margaret Ikpoh, NIHR National Settings Lead for Primary Care and Vice-Chair RCGP and we were joined by Dr Jim Ritchie, Deputy CMO, GM ICB who touched on the role of research in strategic commissioning.
Our GP-Researcher workshops generated thoughtful discussion and were chaired by the GM IRN Steering Group Dr Uwadiae Ima-Edomwonyi, Dr James Higgins and Dr Sinead Millwood. In the CVRM care workshop, Matthew Conroy and Dr Aseem Mishra demonstrated the power of harnessing big data analytics to tackle CVD inequalities. Dr Penny Lewis and Dr Jung Yin Tsang led a thought-provoking workshop on Health Tech and Meds Safety, presenting ample opportunities for collaboration. Dr Sacha Howell and Dr Rebecca Mawson shared their pioneering work to tackle inequities within the fields of breast cancer and women’s health. And Dr Sam Merriel and Dr Hassan Awan led the Men’s Health workshop, sharing their brilliant work in the fields of prostate cancer and Men’s Mental Health.
We thank all of our delegates and speakers for their engaging and enthusiastic contributions to our event. Special thanks to the NIHR GM-ARC team Sue Wood, Joanna Triggs and Carly Rolfe who’s consummate professionalism ensured that the event ran as smoothly as possible. The GM IRN and this event has been funded through the NIHR North West RRDN Strategic Funding Award 2025/2026.
Event Gallery











Event Agenda

Speaker Bios
Dr Maria Ahmed Drake
Director of GM Inclusive Research Network and Principal GP at Manchester Integrative Medical Practice. As a GP serving one the most deprived and diverse populations, Maria is passionate about engaging her patients in research to improve health outcomes and tackle health inequalities. She has acted as Principal Investigator for numerous studies in disease areas including cancer, cardiometabolic disease and mental health and has provided research consultancy for commercial and non-commercial study partners. Her substantive role as Consultant in Primary Care Research, combined with her former roles as GM NIHR GP Research Champion and NIHR GP Academic Clinical Fellow (ACF) have granted her unique insight into the challenge of navigating the provision of high-quality care, with engaging her practice team and patients in research, whilst respecting the needs of researchers working to time and target. Maria holds additional qualifications in patient safety (PhD), public health (MPH), education (SFHEA) and healthcare leadership (MSc) and is a recipient of the prestigious NHS Leadership Academy Senior Healthcare Leadership award. She has held various system leadership and quality assurance roles including as Founding Director of the BMJ award-winning ‘Lessons Learnt: Building a Safer Foundation Programme’; Non-Executive Board Member at NWAS; GMC Education Associate and CQC Specialist Advisor. Currently, she is a Committee Member at NICE (Suspected Cancer Guideline) and was recently invited to serve on the NIHR Predoctoral Award: Primary Care Funding Committee.
Dr Cordelle Ofori
Director of Public Health at Manchester City Council. Cordelle qualified as a doctor from the University of Nottingham, and went on to train and practice as a GP before specialising in public health medicine. Her first-hand experience of the realities of health inequalities as a GP, and her work with charities in the past inspired her passion for improving health equity. She has a special interest in racial health equity and improving health for marginalised communities. She leads work to protect and improve the health of residents in the city of Manchester using data and evidence, and working with the organisations, agencies and sectors that have an impact on people’s health. This includes the development and delivery of ‘Making Manchester Fairer’, the city’s ambition to tackle the unfair and preventable differences in health between different groups of people. The plan focuses on the foundations of good health such as giving children and young people the best start, community power, and reducing the impact of poverty, racism and discrimination on people’s health.
Prof Caroline Mitchell
Professor of General Practice Research, and a General Practitioner. Caroline’s research critiques and addresses equity bias in healthcare through inclusive, participatory methodologies. She co-founded the influential Deep End Research Alliance (DERA), a collaboration of patients/ communities, practitioners, and academics in Yorkshire and Humber, and co-leads a national community of practice for Deep End Research delivery networks. Caroline’s work focuses on co-designing and evaluating complex interventions for primary care, with expertise in qualitative, mixed-methods, and clinical trial methodologies. Her activism advances equitable research partnerships with underserved communities across NHS priority areas including multiple longterm conditions, musculoskeletal medicine, T2 Diabetes Mellitus remission, reproductive health, cardiovascular medicine, cancer screening and care pathways and integration of advanced practitioner roles into primary care teams.
Prof Peter Bower
Lead of the Centre for Primary Care and Health Services Research, which is part of the NIHR School for Primary Care Research, University of Manchester. Peter co-led the NIHR Rose National Evaluation Team (Rose NET). He is an NIHR Senior Investigator, and an Honorary Fellow of the Royal College of General Practitioners. His work has a focus on mental health, multimorbidity, and the evaluation of innovations in service delivery including effective ways of improving management of long-term conditions, with a focus on multimorbidity, the delivery of effective psychological therapies for common mental health problems, and the effective recruitment of patients to randomised trials. Peter collaborates with colleagues at a range of universities in the UK and internationally and his main methodological interests include evidence synthesis, trials and evaluation methodology.
Prof Margaret Ikpoh
GP Partner at Holderness Health. She is the current Royal College of General Practitioners Vice Chair for Professional Development and Training Standards.
Margaret is the practice lead for research and has had previous roles with the NIHR Yorkshire and Humber as a research champion for First5 GPs and AITs. She is the current National NIHR Settings lead for Primary Care and a Trustee for the Faculty of Medical Leadership and Management. She is the former Associate Director for Primary Care for Hull York Medical School and is a GP Trainer. In 2021 she was voted the Fellow of the year at the RCGP Inspire awards. She is the former co-Chair for the regional Primary Care Workforce Group with NHS England & Improvement for the North-East and Yorkshire Regional People Board and is still an active member. In 2022 she was voted one of HSJ’s top 50 most influential Black, Asian and minority ethnic figures in health. In 2024 she was awarded the Caribbean and African Health Network Special Recognition Award for Leadership in Primary Care. In 2024 she was appointed as a Trustee for the Faculty of Medical Leadership and Management. In 2025 Margaret Ikpoh was also appointed as Patron of the Caribbean & African Black Healthcare Awards, in recognition and celebration of her leadership, advocacy, and longstanding contributions to advancing equity within healthcare.
Dr Jim Ritchie
Deputy Chief Clinical Officer (Interim) and Chief Clinical Information Officer for NHS Greater Manchester ICB. He is also a practicing consultant renal physician at the NCA. Jim is dedicated to enhancing research capacity and capability across the entire GM health and care system, ensuring opportunities are equitable and inclusive for all members of our population and staff.
Prof Tom Blakeman
GP and Professor of Primary Care at the Centre for Primary Care and Health Services Research. Tom’s roles include: Principal Investigator for the NIHR Health Services & Delivery Research Programme study: Apply Systems Thinking to enhance recovery after acute kidney injury; (ASTERAKI); Co-Lead and Board member for the NIHR Manchester School for Primary Care Research ; Co-Lead for the NIHR Greater Manchester Patient Safety Research Collaboration Developing Safer Health and Care Systems Theme; Co-Lead for the NIHR Manchester Integrated Academic Training (IAT) Programme.
Matthew Conroy
Matt Conroy is the Analytical Service Lead for Primary Care with NHS Greater Manchester Integrated Care and alumni of the prestigious NHS Graduate Management Training Scheme. He is renowned for his expert knowledge of General Practice data across Greater Manchester and has developed a wide portfolio of analytical tools to support the health and care system. He is passionate about using routinely collected data to identify and reduce health inequalities, and to improve the health and wellbeing of the people of Greater Manchester. Working with clinical colleagues Matt is developing a set of innovative patient centred tools to identify those with the greatest unmet clinical need. The first of these tools, CVNeed, has been shortlisted for two HSJ Awards and Matt’s work on CVNeed was awarded by the British Computer Society with the John Perry Prize in 2024 for innovation and excellence in primary care data. Graduated with a First Class MPhys (Hons) Physics with Mathematics degree from the University of Sheffield in July 2014 obtaining a First in all modules undertaken.
Dr Almas Agha
Primary Care Consultant in CVRM at Manchester Integrative Medical Practice. Almas is a GP Trainer and GP Lead for CVRM at MIMP and has spearheaded the early adoption of cutting-edge treatments in diabetes, obesity and hyperlipidaemia for our patients. She is an experienced GP educator who is regularly imparting her knowledge and skills to fellow GPs and multidisciplinary clinicians. She has given lectures on the management of diabetes, hyperlipidaemia, cardiovascular prevention and COPD. Almas is associated with the British Muslim Heritage Centre and has worked alongside Diabetes UK in delivering lectures to the local community. She was awarded a Champions Muslim Community award for her services to the community in 2022. Almas is a member of the LMC and practice representative for her local PCN.
Dr Jung Tsang
I am a GP (primary care physician) and researcher, with a specialist interest in clinical informatics. My research to date harnesses the increasing availability of health and social care data to improve care quality and reduce inequalities in outcomes. Grounded in an understanding of routine clinical practice, I have training and experience in a range of quantitative, qualitative, public and patient involvement (PPI) and health data science skills. I am currently awarded a NIHR Doctoral Fellowship leading work on exploring how we can address problematic polypharmacy, an increasing global priority. My approach combines large population-based data analysis (CPRD) with stakeholder and patient experiences, seeking to improve our understanding of problematic polypharmacy in primary care. In particular, I aim to develop a measure to improve the identification of problematic polypharmacy through accounting for individual patient factors and clinical diagnoses.
Dr Penny Lewis
Senior Clinical Lecturer in the Division of Pharmacy and Optometry and registered Pharmacist. For over 20 years, Penny has been undertaking research that seeks to understand and improve medication safety and the effective delivery of pharmaceutical care to improve patient outcomes. Penny actively promotes research engagement and fosters the research ambitions of healthcare professionals through her role as Academic Career Development Lead of the National Institute of Health and Care Research (NIHR) Applied Research Collaboration Greater Manchester. Penny is also Equity, Diversity, and Inclusion Lead for the NIHR Greater Manchester Patient Safety Research Collaboration, developing and implementing strategies to reduce safety inequities.
Dr James Higgins
I have been a GP partner at Brinnington Surgery, which serves one of the most deprived populations in GM for 15 years and Clinical Director for Tame Valley PCN since 2019. In addition to this I have been the Named GP for Safeguarding children & vulnerable adults within Greater Manchester ICB covering Stockport since 2015.
Throughout the years in these roles I have always been keen to test new concepts and we have piloted a great number of services & approaches over the year as a practice, including very early pilots around social prescribing. I have to date not been heavily involved in research within primary care but am keen to understand the opportunities available to help learn what approaches and treatments work for deprived populations and to see how practices across a broader footprint (such as a PCN or locality) can better collaborate to help support researchers in identifying and engaging appropriate populations to partake in research.
Dr Hassan Awan
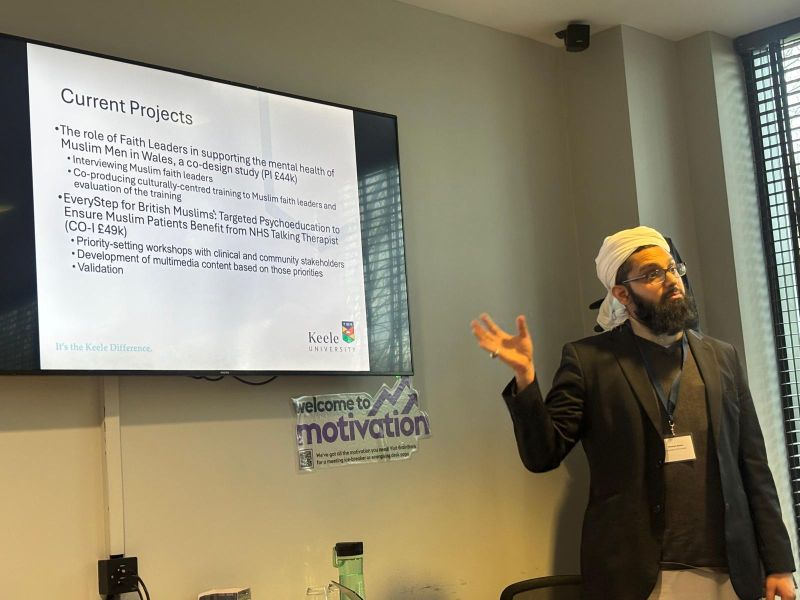
NIHR Clinical Lecturer in Primary Care at Keele University’s School of Medicine and a practicing GP in inner-city Manchester. Hassan’s research focuses on addressing mental health inequalities in underserved communities, with particular expertise in culturally safe approaches that tackle systemic barriers to care. He completed a Wellcome Trust-funded PhD exploring how South Asian men with long-term conditions understand, experience, and seek help for emotional distress, through which he developed the HICCMAT framework for meaningful community engagement in research. Hassan combines clinical practice, academic research, and his role as a community faith leader to bridge the gap between evidence and practice in mental healthcare for diverse populations.
Dr Sam Merriel
NHS GP in North West England and Clinical Senior Lecturer in the Centre for Primary Care and Health Services Research at the University of Manchester. Sam’s main research interests include the prevention and early detection of cancer, understanding and addressing cancer inequalities, and the development and evaluation of new diagnostic tests in primary care. His research portfolio includes studies on prostate cancer diagnosis, proteomic biomarkers for head & neck cancer, GP concordance with cancer diagnosis guidelines, and ethnic differences in blood tests commonly used for cancer detection in primary care. Sam is an Associate editor of the British Journal of General Practice. He served on the National Institute for Health and Care Excellence (NICE) prostate cancer guidelines update committee in 2021, and he has been a member of expert reference groups for Prostate Cancer UK, Movember, the National Cancer Research Institute, and NHS England.
Dr Uwadiae Ima-Edomwonyi
General Practitioner in Hyde, Tameside, Greater Manchester, a GP Educator/Trainer (undergraduate & postgraduate) and an MRCGP SCA examiner. Uwa is the Research Lead for his practice and a member of the Greater Manchester Inclusive Research Network steering group. He is passionate about Medical Education, Leadership, Research and IMG/Peer mentorship and support. He is the Chair of the Northwest England Faculty and a member of the RCGP UK Council. In addition to championing the cause for IMGs, he continues to make widespread positive impact, inspire colleagues and demonstrate exemplary leadership, in the medical profession and beyond.
Dr Sacha Howell
Senior Lecturer and Honorary Consultant in Medical oncology in Manchester. Sacha is director of the Manchester Breast Centre and the Prevent Breast Cancer Research Unit. Clinically Sacha leads the Manchester University NHS Foundation Trust Family History Risk and Prevention Clinic and treats patients with Breast Cancer at The Christie Hospital. His major research focus is in enhancing risk prediction and prevention of breast cancer, in younger women particularly. He has recently completed recruitment to a 1,000-participant risk prediction study (BCAN-RAY) which highlighted very low uptake in women from Black and South Asian communities. A second study (‘Micrima’) successfully recruited 240 women to community-based breast density assessment, with more than 2/3rds from non-White ethnic groups. Acceptability to the approach was high and Sacha is keen to discuss how these findings can now be used to improve access and uptake to risk prediction, screening and prevention in diverse communities.
Dr Rebecca Mawson
NIHR Clinical Lecturer in Primary Care at the University of Sheffield and practicing GP with a focus on addressing reproductive health inequalities through innovative co-design methodologies. Rebecca’s research specifically targets improving healthcare access and experiences for under-represented populations. Her academic career began at the University of Sheffield in 2016, where she was awarded an NIHR In-Practice Training Fellowship in 2018. She completed her MD in 2022, which examined inequalities in sexual and reproductive health in general practice, with particular attention to barriers faced by those in deprived communities. Since beginning her NIHR Clinical Lecturer post in April 2023, Rebecca has expanded her research portfolio to encompass various aspects of sexual and reproductive health, including contraception access for under-represented populations, menopause care, and HIV management in primary care settings. She also maintains special research interests in endometriosis and polycystic ovary syndrome (PCOS). Rebecca is currently leading ‘The Hormone Effect’ (THE), an innovative project funded by the South Yorkshire Digital Health Hub that explores the effects of hormonal contraception through digital tracking methodologies. Her ongoing work includes developing community- led research initiatives where community researchers facilitate focus groups with women from ethnic minority backgrounds to better understand their experiences with contraception services.
Dr Sinead Millwood
GP Research Lead at Hawthorne Medical Centre and GM IRN Steering Group member. Sinead qualified as a GP in 2021. She works for Hope Citadel, a community interest company in Manchester running GP practices in areas of deprivation. She is passionate about women’s health, campaigning for clean air and bringing research to deprived populations.
Susan Neeson
Director of Operations NIHR North West Regional Research Delivery Network
A senior healthcare and clinical research leader with a research nursing background and over 20 years’ experience delivering complex clinical trials across the UK health and life sciences landscape. Currently Operations Director for the NIHR Regional Research Delivery Network North West, providing strategic oversight of large-scale research delivery services, governance, and business operations, including budgetary responsibility and leadership of multidisciplinary teams across multiple NHS partners. Extensive experience in research system transformation and building high-performing teams, with a proven track record of leading major organisational change. This includes playing a key leadership role in the transition to the Regional Research Delivery Network and workforce transformation, supported by a national role within the RDN. Passionate about improving patient access to research and promoting the North West’s research capability and contribution to UK life sciences.
Joanne Henry
Head of Research Delivery & Support for Wider Care Settings. A Children and Young People’s Nurse by background but have worked in research delivery for the last 7 years within the former National Institute for Health and Care Research (NIHR) Clinical Research Network (CRN), now NIHR Research Delivery Network. My research experience includes both non-commercial and commercial delivery, across a variety of specialities and settings including NHS and non-NHS. I now lead an incredible team of clinical and non-clinical staff, taking research out into wider care settings across the North West including primary care, residential care and community settings, and finding novel ways to increase inclusion and diversity in research. I am part of a national Agile Research Delivery group driving forward transformation of research delivery in the UK with a particular focus on increasing research capacity and capability within wider care settings.
Dr Omair Razzaq
A GP Partner at Ashton Medical Group – a research-active practice committed to offering patients access to high-quality academic and commercial studies. I worked closely with the previous CRN: GM as a research-active GP and as Primary Care Specialty co-Lead. I have helped increase GP practice participation across the region and have developed a GP Integrated Training Post in research in Tameside. I am passionate about integrating research into routine practice, mentoring colleagues and providing more opportunities to all patients. Now co-Director of the Greater Manchester Primary Care Commercial Research Delivery Centre I am supporting the growth of commercial research within our region to ensure our patients have access to cutting edge technology and treatments.
